MINNETONKA, Minn.--(BUSINESS WIRE)--UnitedHealthcare has expanded its efforts to help address the connection between dental care and the opioid epidemic, introducing a public toolkit with information to help support oral health care professionals and patients, especially after wisdom-teeth removal for teens and young adults.
The toolkit — available here — provides information for oral health professionals and all consumers, including an educational flyer with commonly asked questions related to opioids and a checklist to help people better understand pain-management options before and after wisdom-teeth removal.
The toolkit builds upon a companywide approach to address the epidemic from all angles, including dental care. This comprehensive approach includes a pharmacy policy, outreach to dental health professionals and plan participants, along with TV and radio public service announcements (PSAs).
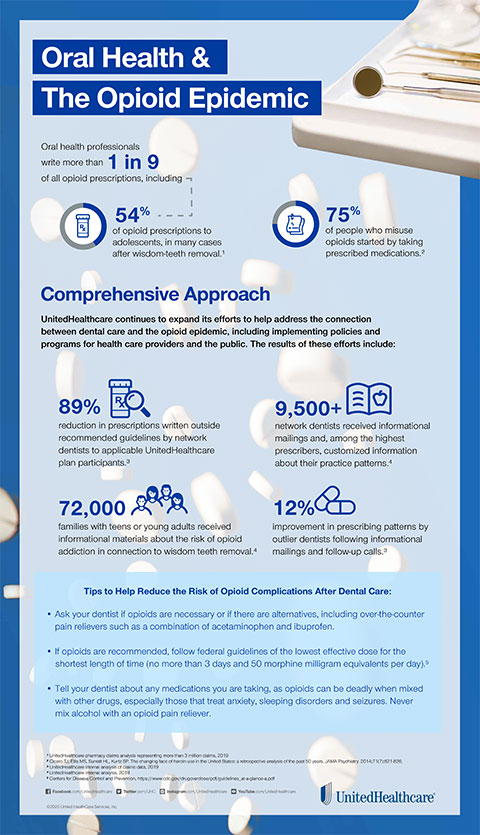
Taken together, these efforts to date have resulted in an 89% reduction in opioid prescriptions above federal guidelines written by network dental health professionals for UnitedHealthcare dental plan participants age 19 and under.1
“Confronting the opioid epidemic requires a comprehensive approach involving multiple stakeholders across the health care system, including addressing the often overlooked connection with dental care,” said Tom Wiffler, CEO, UnitedHealthcare Specialty Benefits. “Working together, these initiatives are making a meaningful difference in helping address this important national public health issue.”
The opioid epidemic causes more than 130 overdose deaths2 each day, while the economic cost exceeds $500 billion annually, according to a study from The Council of Economic Advisors. In addition, oral health professionals write 12% of all opioid prescriptions, including more than 54% of opioid prescriptions for adolescents3 – an age group especially vulnerable to addiction.4
UnitedHealthcare’s comprehensive approach to combating opioid use related to dental care also includes:
- Pharmacy Policy: The policy change — enacted in late 2018 — capped at three days and fewer than 50 morphine milligram equivalents per day for all first-time opioid prescriptions written by UnitedHealthcare network dental health professionals for people age 19 and under, as recommended by the Centers for Disease Control and Prevention (CDC). Among the first dental plans to take this step, the policy was designed to help limit access to often unnecessarily large prescriptions and help facilitate patient engagement to reduce the risk of misuse.
- Dental Health Professionals: Network dental health professionals identified as consistently prescribing opioids above CDC guidelines — as measured by the number of days per supply and/or morphine milligram equivalents per day — will receive information about their status and access to the pain-management toolkit to share with patients. Following similar UnitedHealthcare outreach last year to more than 2,800 oral health professionals, prescribing patterns improved by 12%.1
- Dental Plan Participants: Nearly 72,000 UnitedHealthcare dental plan participants with dependents ages 16 to 22 received information by e-mail about the risks associated with opioids, specifically in connection with wisdom-tooth extractions. More than two-thirds (70%) of wisdom-tooth extractions for people ages 16 to 22 result in at least one opioid prescription,3 so providing this information is designed to help parents and young people better identify pain management alternatives and strategies to manage the frequency of use, dosage and proper disposal of unused opioids. A recent study from Stanford University found that teens and young adults can end up in a battle with opioid addiction following wisdom-teeth removal.
- Public Service Announcements (PSAs): TV and radio PSAs — in collaboration with Shatterproof, a national nonprofit organization dedicated to reversing the addiction crisis in the United States — last year aired on nearly 400 stations across the country, helping parents and health professionals understand the connection between oral health and the opioid epidemic.
UnitedHealthcare, a UnitedHealth Group (NYSE: UNH) company, is also collaborating with health care providers and communities and using powerful data and analytics to prevent opioid misuse and addiction, tailor ways to treat people who are addicted and support long-term recovery.
Learn more about what UnitedHealthcare is doing to address the opioid epidemic.
About UnitedHealthcare
UnitedHealthcare is dedicated to helping people live healthier lives and making the health system work better for everyone by simplifying the health care experience, meeting consumer health and wellness needs, and sustaining trusted relationships with care providers. In the United States, UnitedHealthcare offers the full spectrum of health benefit programs for individuals, employers, and Medicare and Medicaid beneficiaries, and contracts directly with more than 1.3 million physicians and care professionals, and 6,500 hospitals and other care facilities nationwide. The company also provides health benefits and delivers care to people through owned and operated health care facilities in South America. UnitedHealthcare is one of the businesses of UnitedHealth Group (NYSE: UNH), a diversified health care company. For more information, visit UnitedHealthcare at www.uhc.com or follow @UHC on Twitter.
1 UnitedHealthcare pharmacy claims analysis, 2019
2 2 CDC/NCHS, National Vital Statistics System, Mortality. CDC Wonder, Atlanta, GA: US Department of Health and Human Services, CDC; 2018. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
3 UnitedHealthcare pharmacy claims analysis representing more than 3 million claims, 2019
4 Pediatrics February 2019, 143 (2) e20182752; DOI: https://doi.org/10.1542/peds.2018-2752