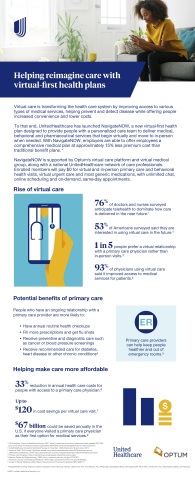
MINNETONKA, Minn.--(BUSINESS WIRE)--UnitedHealthcare, a UnitedHealth Group (NYSE: UNH) company, announced the launch of NavigateNOW, a virtual-first health plan that offers an integrated approach to provide care both virtually and in-person. Through this new health plan, eligible UnitedHealthcare members will be able to receive various types of care, including wellness, routine, chronic condition management, urgent and behavioral health services, wherever they are.
Starting this year for select employers in nine markets, NavigateNOW will provide people with a comprehensive medical plan that offers a simpler, more convenient experience at approximately 15% less premium cost than traditional benefit plans. People in the NavigateNOW plan will receive 24/7 access to a personalized Optum care team for primary, urgent and behavioral health care services, backed by a national UnitedHealthcare network of care professionals.
“By collaborating with Optum, UnitedHealthcare is developing a more integrated and coordinated health care system that uses technology and personal support to help encourage whole-person health, which may help prevent and detect disease before it starts,” said Dr. Rhonda Randall, chief medical officer, UnitedHealthcare Employer & Individual. “UnitedHealthcare and Optum will continue working together to modernize our approach to health benefits and care delivery, using technology and data to help make it more convenient for our members to access various types of medical care to support their physical and mental well-being.”
Enrolled members will pay $0 for virtual and in-person primary care and behavioral health visits, virtual urgent care and most generic medications, with unlimited chat, online scheduling and on-demand, same-day appointments. NavigateNOW members also gain access to a wearable device well-being program that enables people to earn more than $1,000 per year by meeting certain daily activity targets, including for walking, cycling, swimming and strength training (among dozens of others).
NavigateNOW is being offered to employers in the following markets: Little Rock, Ark.; Fort Meyers, Fla.; Pittsburgh; Springfield, Mass.; Minneapolis/St. Paul, Minn.; Richmond, Va.; Indianapolis; Dallas; and Houston.
Enrolled members in NavigateNOW will be able to complete a health profile to indicate personal preferences, current medications and existing health conditions. Based on the assessment, each member is matched with a personalized care team, which may include a board-certified physician and other care providers who will work together to deliver primary, urgent and behavioral health care. This care team is led by a dedicated primary care provider who will virtually deliver care and seamlessly connect the individual to in-person Optum providers and other health professionals when necessary. The integrated care model is designed to identify health issues earlier, promote the use of preventive care, and deliver whole-person care in the most appropriate setting.
For instance, during virtual primary care appointments, Optum providers will have the ability to connect the UnitedHealthcare member with behavioral health services within the virtual platform as needed. This will help facilitate additional virtual or in-person behavioral health appointments, including therapy, medication management and additional care coordination with other health services.
“Patients want more options for getting care that is convenient for them and their lives,” said Kristi Henderson, Optum senior vice president for digital transformation, and CEO of Optum Virtual Care, which includes Optum’s national virtual-first medical group. “Our work with UnitedHealthcare is designed to help make it simpler for patients and members to interact with their care providers by bringing together our digital resources and national clinical footprint to provide a more seamless, connected experience.”
NavigateNOW is supported by Optum’s new virtual care platform and virtual medical group, which helps bring simplicity to getting care whenever and wherever it is needed. The proprietary virtual care platform enables UnitedHealthcare members to schedule appointments online and provides multiple ways for them to communicate with their care team, such as live chat and video visits. If after a virtual visit a member needs additional health services, such as for a procedure or an X-ray, the care team can use the platform’s precision navigation tools to help connect the individual to a care provider in UnitedHealthcare’s national network, including over 1,600 facilities in Optum’s national ambulatory provider network.
NavigateNOW is the latest of several UnitedHealthcare virtual care offerings supported by the Optum virtual care platform and other national telehealth providers. These expanded virtual care services are part of broader efforts by UnitedHealthcare and Optum to help enable people to use technology to access high-quality care at a lower cost.
About UnitedHealthcare
UnitedHealthcare is dedicated to helping people live healthier lives and making the health system work better for everyone by simplifying the health care experience, meeting consumer health and wellness needs, and sustaining trusted relationships with care providers. In the United States, UnitedHealthcare offers the full spectrum of health benefit programs for individuals, employers, and Medicare and Medicaid beneficiaries, and contracts directly with more than 1.3 million providers and care professionals, and 6,500 hospitals and other care facilities nationwide. The company also provides health benefits and delivers care to people through owned and operated health care facilities in South America. UnitedHealthcare is one of the businesses of UnitedHealth Group (NYSE: UNH), a diversified health care company. For more information, visit UnitedHealthcare at www.uhc.com or follow @UHC on Twitter.