LOUISVILLE, Ky.--(BUSINESS WIRE)--Humana Inc. (NYSE: HUM) today announced it has implemented a Clinical Quality Metrics Alignment (CQMA) program to streamline and standardize the set of clinical quality metrics used for physicians.
The program will support physicians who are participating in value-based payment relationships with Humana. In addition, the reduction of clinical measures will also help physicians, currently in fee-for-service agreements with Humana, in their transition to value-based care.
According to a 2015 survey conducted by the American Academy of Family Physicians and sponsored by Humana, 61 percent of family physicians receive payment from seven or more health plans, which can lead to excessive, inconsistent and overlapping quality reporting requirements. These requirements may contribute in part to the fact that 49 percent of U.S. physicians meet the standard definition of professional burnout. To reduce the burden on physician practices, which spend more than $15 billion annually on quality reporting, greater standardization of metrics and more efficient reporting processes are needed.
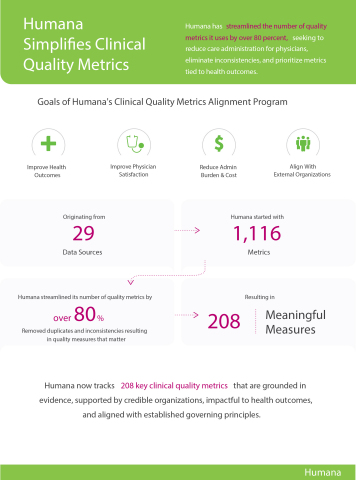
To address this issue, Humana’s CQMA program collected 1,116 quality metrics from 29 different data sources across the company, and vetted these metrics for duplicates, inconsistencies, and clinical relevance. Following extensive refinement and analysis, which included input from physician stakeholders, Humana has consolidated the 1,116 metrics previously used into a set of 208 key quality metrics—an 80-plus percent reduction. The streamlined set of metrics emphasizes improving patient health outcomes, and is aligned with broader industry efforts to standardize measures used to evaluate clinical quality.
This coordinated effort follows the February 2016 introduction of Core Quality Measures by America’s Health Insurance Plans (AHIP), in collaboration with its member plan chief medical officers, leaders from the Centers for Medicare and Medicaid Services (CMS) and the National Quality Forum (NQF), as well as national physician organizations. These were introduced to ensure the adoption of meaningful, efficient, payer-agnostic quality measures across the industry. Humana’s CQMA program has consolidated metrics in alignment with such efforts to address physician pain points around quality reporting, lower reporting costs and maximize the impact of metrics on improving patient health.
“At Humana, we are committed to helping physicians succeed in their transition from fee-for-service to value-based care,” said Roy Beveridge, MD, Chief Medical Officer at Humana. “Metrics that are not connected to patient health can serve as obstacles in their transition and distract from the intent of care tied to quality. Through our CQMA program, we hope to greatly simplify quality reporting and alleviate physician burdens.”
“Measuring and managing quality is key in Iora Primary Care's work to continually improve the value of care delivered to our older adult patients,” said David Gellis, MD, Vice President of Clinical Performance and Development for Iora Health. “Humana's leadership in this area allows us to focus on measures that matter to patients and clinical outcomes, rather than the measurement system. Overall, this initiative recognizes the value of Iora's relationship-based care model.”
In 2015, Humana members cared for by physicians in value-based relationships experienced healthier outcomes, including 6 percent fewer emergency room visits than members in standard Medicare Advantage settings, as well as higher screening rates for colorectal cancer screening (+8 percent), breast cancer screening (+6 percent) and osteoporosis management (+13 percent).
Approximately 1.8 million of Humana’s individual Medicare Advantage members are cared for by approximately 49,600 primary care physicians in more than 900 value-based payment relationships across 43 states and Puerto Rico. For more information, visit humana.com/valuebasedcare.
About Humana
Humana Inc., headquartered in Louisville, Ky., is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care. The company’s strategy integrates care delivery, the member experience, and clinical and consumer insights to encourage engagement, behavior change, proactive clinical outreach and wellness for the millions of people we serve across the country.
More information regarding Humana is available to investors via the Investor Relations page of the company’s web site at www.humana.com, including copies of:
- Annual reports to stockholders
- Securities and Exchange Commission filings
- Most recent investor conference presentations
- Quarterly earnings news releases
- Calendar of events
- Corporate Governance information